Small Intestine: Crohn’s Disease
Crohn’s Disease
Basics
- Inflammatory Bowel Disease (IBD) – Chronic Inflammatory Disease of the GI Tract
- Almost Half of Patients Require Surgery Within 10 Years of Diagnosis
- Smoking Increases Risk of Development
- Surgery is Not Curative
- 10-12-Fold Risk of Small Bowel Adenocarcinoma
Inflammation
- Can Occur Anywhere Along the GI Tract from Mouth to Anus
- Skip Lesion Non-Continuous
- Most Common Location: Terminal Ileum
- Inflammation in Full-Thickness/Transmural
- Normal Surrounding Mucosa
Presentation
- Three-Main Presentations:
- Inflammatory – Tender Sites of Inflammation
- Fistulizing – Abscess or Fistula
- Fibrosing – Submucosal Fibrosus, Strictures & SBO
- General Sx:
- Vague Abdominal Pain – Most Common Initial Presentation
- Nausea, Vomiting & Diarrhea
- Hematochezia
- Anorexia & Weight Loss
- Malnutrition & Fatigue
- Earliest Lesion: Aphthous Ulcers
- Most Common Anal Lesions: Skin Tags #1 & Fissure #2
- May See B12 Deficiency (TI Involvement Prevents Absorption)
Extraintestinal Manifestations
- Arthritis – Most Common Extraintestinal Manifestation
- Anterior Uveitis or Iritis
- Rash – Erythema Nodosum or Pyoderma Gangrenosum
- Kidney Stones
- Type: Calcium Oxalate & Uric Acid
- Cause of Calcium Oxalate Stones: Decreased Oxalate Binding to Calcium
- Due to Steatorrhea with Increased Intraluminal Fat Binding Calcium
- Causes Increased Oxalate Absorption in the Colon & Release in Urine
- Primary Sclerosing Cholangitis
- Much More Highly Associated with Ulcerative Colitis than Crohn’s Disease
Diagnosis
- Imaging (CT or MRI)
- Colonoscopy with Intubation of Terminal Ileum & Mucosal Bx
- Morphology:
- Ulceration & Fissure
- Cobblestone Mucosa – Chronic Ulcer Coalescence Causing Ulceration Around Normal Appearing Nodular Mucosa
- Creeping Fat/Fat Wrapping – Mesenteric Fat Wraps Around the Bowel Wall with Thickening
- Pathognomonic
- Noncaseating Granulomas
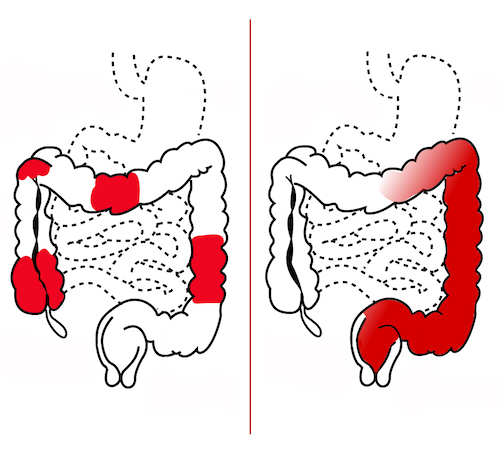
Skip Lesions of Crohn’s (Left) Compared to Continuous Lesion of UC (Right) 1

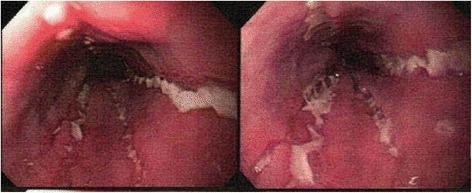
Cobblestone Mucosa of Crohn’s 2

Creeping Fat of Crohn’s 3
Serpiginous Ulcers of Crohn’s 4
Crohn’s Disease – Treatment
Medical Treatment
- Acute Flare: Steroids (Budesonide or Prednisone)
- If Oral Steroids Fail Admit for IV Steroids
- Steroid Resistant Disease: Infliximab (Remicade/TNF-α Inhibitor)
- Fistulas or Perianal Disease: Steroids & Infliximab
- Infection Control: Cipro/Flagyl
- Maintenance:
- Mild Active Disease: 5-Aminosalycylic Acid (Sulfasalazine/Mesalamine)
- Remission: Infliximab
Surgery Indications
- Primary:
- Perforation
- Cancer
- If Refractory to Nonoperative Managements:
- Abscess
- Fistula
- GI Bleed
- Stricture/SBO
- Intractable Pain
- Growth Retardation
Surgery – General Considerations
- Most Common Surgical Procedure in Crohn’s Disease: Bowel Resection
- Stricturoplasty is Becoming More Prominent
- Contraindications to Stricturoplasty:
- Active Sepsis
- Perforation
- Phlegmon or Abscess
- Severe Malnutrition
- Concern for Dysplasia or Malignancy
- Contraindications to Stricturoplasty:
- High Postoperative Recurrence Rates
- Endoscopic Recurrence: 80% at One Year
- Clinical Recurrence: 10-15% Per Year
Surgical Treatment
- Duodenal Disease:
- Preferred Method: Stricturoplasty
- If Inaccessible or Too Complex: Gastrojejunostomy
- If Preoperative Gastric pH Acidic: Include Vagotomy to Avoid Marginal Ulcers
- Avoid Vagotomy if Gastric pH Normal – Risk for Dumping Syndrome
- May Consider a Duodenojejunal Bypass if Structure Distal to Second Portion
- If Preoperative Gastric pH Acidic: Include Vagotomy to Avoid Marginal Ulcers
- Small Bowel (Jejunum & Ileum) Disease:
- Preferred Method: Stricturoplasty (Include All Areas of Stricture)
- If Unable to Preserve Bowel: Resection
- If Only a Single Short Segment is Present: Consider Resection
- Should Question Dx
- If Diffuse Jejunoileitis: Combination Stricturoplasty, Resection & Conservation
- Very Difficult & Requires Careful Consideration/Judgment
- If Inflammatory Mass Would Require Too Extensive a Resection: Consider Proximal Stoma & Delay Further Surgery Until Some Inflammatory Regression Has Occurred
- Colonic Disease:
- Limited Disease: Segmental Colectomy
- Diffuse Colorectal Disease: Proctocolectomy & End Ileostomy
- Resect 2 cm Beyond Visible Disease
- Do Not Preform a Restorative Ileal Pouch Anal Anastomosis (IPAA) – High Risk of Failure
- Toxic Megacolon: Total Colectomy & End Ileostomy
- Anorectal Disease:
Inflammatory Bowel Disease (IBD) Comparison
Ulcerative Colitis (UC)
Inflammatory Bowel Disease Type Unspecified
Comparison
References
- Wikimedia Commons. (License: CC BY-4.0)
- Ye Z, Lin Y, Cao Q, He Y, Xue L. Granulomas as the Most Useful Histopathological Feature in Distinguishing between Crohn’s Disease and Intestinal Tuberculosis in Endoscopic Biopsy Specimens. Medicine (Baltimore). 2015 Dec;94(49):e2157. (License: CC BY-4.0)
- Kaiyasah H. Crohn disease – creeping fat sign (gross pathology). Radiopaedia.org. rIR 46655
- Nathoo S, Hood WA, Keihanian S, Collinsworth AL, Glover SC. Tofacitinib for the treatment of tumor necrosis factor-α inhibitor refractory esophageal Crohn’s disease: a case report. J Med Case Rep. 2016 Sep 23;10(1):264. (License: CC BY-4.0)